During medical school, we are in the privileged position to explore a specific medical speciality within any country in the world – known commonly as a medical elective. All universities schedule the elective at different times, but usually during the final two years of medical school, with the duration tending to vary between one to two months. My school (Hull York Medical School) assigns our medical elective during the summer before the start of our final year. A perfect time for hot weather and higher travelling prices!
Although the elective begins in Year 5, I recommend you start thinking about it at the beginning of Year 4 (trust me planning a life changing trip takes time). I think it is important to begin by reflecting on what you really want to achieve from your medical elective. It is a unique opportunity to grow as a person and a professional. You may see this time as a chance to develop in research, experience a niche speciality or to travel the world. Personally, I have always known that I wanted to return to The Philippines during my elective, as I fell in love with the country and its culture during my Gap Year travels before medical school. Furthermore, I had six weeks to complete my elective and I knew four weeks would curb my need for travel and adventure, so I chose to divide my elective into two: four weeks within The Philippines and two weeks in the UK. I have a keen interest to pursue a career in Plastic surgery, so I chose to spend the final two weeks in the UK advancing my surgical portfolio by shadowing the Plastics team at a Regional Burns Unit Hospital.
When planning an elective abroad there are two options; you can reach out to supervisors from hospitals abroad and plan the elective yourself or you can use a package deal company. Planning the elective yourself tends to work out cheaper but it entails considerably more work, is often independent and does not provide the security of the company. Personally, I chose the package company for ease and safety, with the added bonus of living in a large house of other students from around the world for social events and forming new friendships. Again, with both options, make sure to start early as an elective abroad involves extra organising such as travel vaccines (a must!), flights, accommodation, and travel insurance.
The Philippines, a developing country, is an archipelago consisting of more than 7,000 islands at constant threat from natural disasters. The Philippines was colonised by the Spanish in 1500s, and the country remains divided between Catholics and Muslim communities. The Central Visayan Islands consisting of Bohol/Cebu/Leyte/Masbate/Negros/Panay/Samar have reputations of being the safest areas to travel. I lived on Panay Island in Iloilo City, in the organisations’ sizeable house for 50 students. The atmosphere within the house was riveting, with communal meals and daily activities to relish. Whilst on placement, I worked at the Western Visayas State University Hospital within the surgical department. The Filipino healthcare is private with a social services system called PhilHealth, which covers the cost of overnight stay and some minor surgeries for patients of lower socioeconomic backgrounds. The hospital system differs from the UK with patients being assigned to medicine or surgery as soon as they enter the hospital. The surgical team primarily work within the emergency department (ED) to triage and treat patients, with most patients remaining in ED for an average of three days. There was one surgical ward for the entire hospital and most patients on the ward were post-operative cholecystectomies or were being monitored for the highly prevalent colorectal cancer. During my placement, I followed the final year medical students whose responsibilities are the equivalent to our Foundation Year Doctors. The students work every day on a four-day rotation which includes a full 36-hour shift receiving no pay. Ironically during my elective placement, doctors in the UK were striking for better working conditions (deserved) whilst I found myself experiencing unimaginable working conditions.

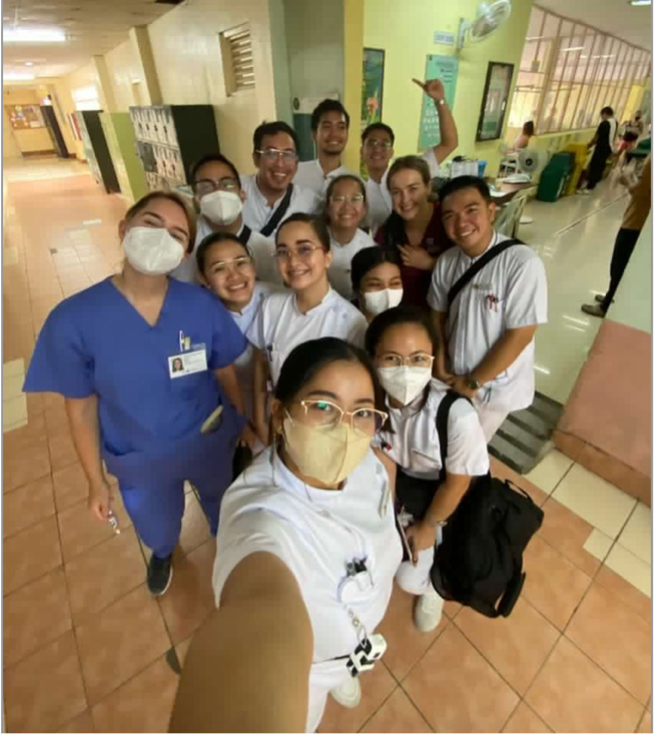
My typical week consisted of four days in the hospital, tending to finish at 2pm due to the heat and distressing nature of the placement. Most days I attended handover, a teaching session, ward round and scrubbed into surgery on surgical days. I assisted in multiple laparoscopic cholecystectomies and sympathised with the consultant surgeons who had to reuse the single-use laparoscopic instruments, persisting with a broken laparoscopic camera which kept having to be placed in a ‘Starbucks’ flask of hot water to remove the condensation. The surgery was easily four times the length of one I assisted on one of my UK placements. However, the staff within the theatre encouraged a positive atmosphere and laughs were had all around. Nevertheless, the unsurmountable pressure on their healthcare system was grossly evident, and the system I found myself in shocked me daily.
Outside of placement, I used the opportunity to recharge my batteries by relaxing at the beach or exploring the island fruit markets and many shopping malls. Every weekend, myself and a small group of other students from the house travelled and explored the surrounding islands. Getting adventurous, we swam with whale sharks, completed canyoneering (avoid if you are afraid of heights) and hiked waterfalls. The Philippines was a unique opportunity to study medicine and experience a new culture whilst exploring a beautiful country.


Once home from The Philippines, I attended a two-week placement at Yorkshire’s Regional Burns Unit. Fortunately, I already had contacts within the Plastic surgery team and was able to organise a shadowing contract with the hospital’s HR department. One top tip: complete this contract in advance to avoid overlap with the Junior Doctor start dates as their contracts take priority! It takes longer than you first anticipate as you will need a DBS check and occupational health assessment for a hospital outside of your medical school. I was able to find accommodation near the hospital and have since been able to claim back this cost using the NHS Bursary (consider the benefits of the NHS Bursary as it makes electives more affordable). I chose to attach mainly to the Burns team day to day, as this is a special interest to me. My days varied between ward time, multidisciplinary team (MDT) meetings, clinics, and lots of theatre time! My biggest achievement was helping manage a patient with a 10% Total Body Surface Area (TBSA) facial and neck burn who was admitted to the hospital on my first day. I followed the patient’s case from resuscitation to debridement and assisted with the skin graft. Upon discharge, the patient had no lasting complications and their graft had 100% uptake, ready to be reviewed in three months at the complex scar clinic. In my two-week placement, I assisted in 20 surgeries for burns and trauma, being entrusted to debride burns and closing wounds with multiple suture techniques. My advice here would be to record any surgeries you attend in your eLogbook! Also, collate the surgical information in a letter and ask a consultant to sign these off to have a record for your portfolio. When spending time within a UK placement, make sure to ask if there are any additional projects you can join to help improve your portfolio. If you find a helpful and encouraging consultant or registrar, make sure to get their contact details and if you feel brave – propose a project to them!
I am extremely pleased with the experience I had during my medical elective, where I tailored my six weeks to ensure I had travel, adventure, and portfolio growth. On reflection, the placement during my time at The Philippines was graphic and challenging, whilst my placement in the UK was engaging and self-promoting. During my Gap Year, I completed a clinical placement abroad and have always reflected on how fortunate we are in the UK with the NHS system, but I also have always understood how few people in the UK appreciate this. I knew returning to The Filipino healthcare would reinforce these feelings, however, I struggled more than I expected I would. Returning to The Philippines, now having experienced working within the NHS setting and myself having complained about the working conditions, sparked a feeling of guilt towards the Filipino staff. Watching the Filipino professionals fight to sustain life in a fragmented system was painful, worse was knowing I could leave their hospitals and never had to work in those conditions myself. It reminds me of the privileged position all UK citizens are in by just having been born in a developed country. It reignites a fight in me to appreciate and progress the NHS. I believe having an experience such as this during medical school is invaluable and would recommend challenging yourself and do something similar if you ever have the opportunity.
~~~~~~~~~~~~~~~~~~~

Sabrina Poppy Barnes is a final year medical student at Hull York Medical School with an interest in pursuing a career within Plastic Surgery and has a special interest in Burns and Reconstruction. In her spare time, she enjoys traveling, cooking and plays lacrosse team sport.

