On the 7th of March, my friends and I had the opportunity to attend the 18th annual British Association of Plastic Reconstructive and Aesthetic Surgeons (BAPRAS) Undergraduate Conference held at Austin Court, Birmingham. The event was organised by a great mix of experienced consultants, registrars and medical students which resulted in a buffet experience of the different flavours of Plastic and Reconstructive surgery, tailored at the right level to encourage interest and enthusiasm.
We arrived early to explore some of Birmingham’s city centre, capturing glimpses of the famous Bullring and Grand Central Station as well as the eye-catching Library of Birmingham before we arrived at the venue. There, we approached the citadel that is the International Convention Centre (ICC); a grand, towering building overlooking the canal and nearby businesses. We entered and, as expected, the interior far surpassed the exterior and the excitement of being in such a beautiful place for the conference could be felt to our cores! To our amusement, when we double checked our emails, we realised that the conference was to be held in Austin Court, a smaller venue opposite the ICC. However, our enthusiasm could not be suppressed as we waited eagerly for the series of lectures to begin in a venue that felt uniquely homely.
“You can only take from Paul to give to Peter if Paul can afford it”
The morning started with an introduction to Plastic and Reconstructive surgery with a brief history lesson on where it all started. Keeping things simple was the motto of the introduction with Mr Dean Boyce, Consultant Plastic and Hand surgeon based in South Wales, quoting that essentially plastic surgery was a “hole filling service” with the key element in the speciality being “you can only take from Paul to give to Peter if Paul can afford it”. This illustrated the basis that you can only take tissue from one area of the body for the use of treating another only if that original section can afford to lose that tissue. This was in reference to the common use of skin grafts and free flaps for reconstruction and restoration of function following trauma.
So how did it all begin? Sir Harold Gillies, commonly known as the father of Plastic surgery, formed a surgical specialty born from the tragedy of war, with the aim to restore form and function to those afflicted with war injuries. Gillies created a famous procedure called the pedicle flap, which took tissue from the forehead to restore the missing tissue from the nose, after an enemy soldier took the phrase “got your nose” a little too literally!
As the lectures progressed, one particular advancement that I was keen to learn more about was the highly advanced Targeted Muscle Reinnervation used in prosthetic arms as mentioned by Mr James Baden, Lieutenant-commander and Consultant Plastic surgeon based in Birmingham. It was amazing to see that with the innervation of the chest muscles, a mechanical prosthetic could restore functions of grip and movement to a soldier who had lost an arm to the war. It is incredible that we have reached this stage already and I think that with further collaborations with the medical and engineering industries, the future in reconstruction will develop to new heights, possibly reaching the realms of science fiction!
Following a short break with refreshments, more lectures focusing on limb, hand, breast, head, neck surgery and reconstructive research took place. Among these, the talk that piqued my interest the most was the hand surgery lecture by Mr Boyce. He discussed various surgical procedures including the use of a free flap-tissue layer on the side of the head to recover the back of the hand. Mr Boyce, as well as the other lecturers, highlighted how this specialty involved the incredible manipulation of the human body for its own recovery, with the simple idea of taking a piece from a healthy area to assist recovery in a damaged area of the body. When I thought about the experiences of my youth; using Play-Doh and interchanging limbs on my action figures who had suffered the injury of excessive playing, I felt that I could closely relate to the creative process involved in reconstructive surgery.
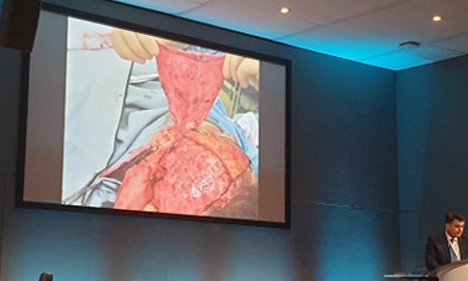
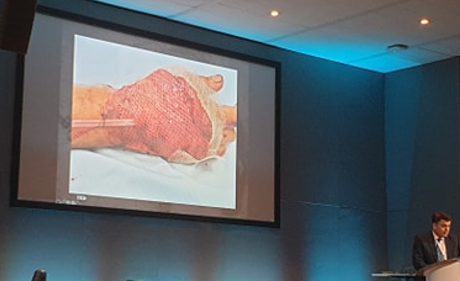
The inventive use of free flaps and novel procedures really highlights how science and artistry go hand in hand in surgery. Another excellent example of this was the use of the bones in the lower leg to replace a part of the jaw, which was mentioned by Mr Demetrius Evrivades, a Consultant Plastic surgeon based at Queen Elizabeth hospital in Birmingham. The key message delivered to the delegates was that as a Plastic surgeon, you must have an element of creativity and enthusiasm for innovation. With each case presented subsequently, lecturers walked us through their thought processes to show us the creativity, flexibility and confidence required in the field of Plastics.
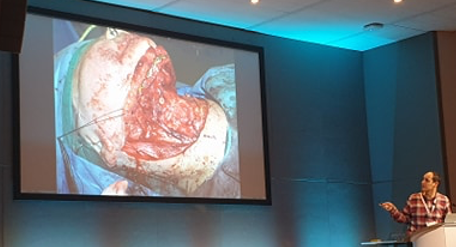


A case I also want to highlight within that series of lectures was the treatment of a patient with Crouzon syndrome. Crouzon syndrome is a genetic condition resulting in facial deformities due to premature craniosynostosis. This condition can result in facial shape changes, vision problems and can cause cerebellar symptoms due to herniation through the foramen magnum. Mr Hiroshi Nishikawa, Consultant Plastic surgeon and clinical lead in the craniofacial unit in Birmingham Children’s hospital, described the use of Fronto-facial Monobloc advancement treatment in a patient with Crouzon syndrome. The premise of this ground-breaking treatment is to alleviate the intercranial pressure from a growing brain and to correct the facial deformities by breaking the bones of the skull across a plane and to extend by a few millimetres. There is an extensive frame used to maintain the advancement and this procedure is repeated over years to reshape the head and correct the deformity. This work was not done by Plastic surgeons alone, Mr Nishikawa emphasised the value of the multi-disciplinary team of Maxillofacial, Neurological and ENT surgeons among the other healthcare staff involved in the care of the patient, working together for the benefit of the patient.
We rounded the event off with the surgical workshop where we had the opportunity to practice and learn the variety of wound closing techniques including Z plasty and rhomboid flap. The Z plasty technique is used to change the orientation of a wound, usually to fit in with natural lines of the face, while the Rhomboid flap is often used in skin cancer due to its versatile nature and use of the surrounding tissue to essentially hide the wound in clear sight.
Despite an exhausting day, we thoroughly enjoyed the BAPRAS 18th Undergraduate Conference and I would definitely recommend this event to other university students. Those who have an interest in the science and the aesthetics of the human body will reap the rewards of the experience at the annual BAPRAS event next year.

~~~~~~~~~~~~~~~~~~~

Bilal Qaddoura is a fourth year medical student at HYMS and the current President of the York Surgical Society. He has a keen interest in trauma surgery as well as a special interest in dermatology. In his spare time, he enjoys salsa dancing and travelling.

